Health
Public health officials confirm second case of Monkeypox identified in Wales

A SECOND monkeypox case has been identified in Wales, public health officials have said today.
Yesterday the UK Health Security Agency (UKHSA) said 18 new cases have been identified in the UK, bringing the total to 225 cases in the UK as of 2 June.
Monkeypox – which is usually found in west and central Africa – has been on the increase during the past month with more than 200 confirmed cases recorded in Britain, Portugal, Spain and the United States.

Anyone can get monkeypox. Currently most cases have been in men who are gay, bisexual or have sex with men, so it’s particularly important to be aware of the symptoms if you’re in these groups
Dr Graham Brown, Consultant in Communicable Disease Control for Public Health Wales, said: “Public Health Wales is today (3 June) confirming that an additional case of monkeypox has been identified in Wales. This brings the total in Wales to two.”
“We are working with the UK Health Security Agency (UKHSA), Public Health Scotland, and Public Health Agency Northern Ireland, and we are ready to respond to cases of monkeypox in Wales.
“The case is being managed appropriately. To protect patient confidentiality, no further details relating to the patient will be disclosed.
“We are reassuring people that monkeypox does not usually spread easily between people, and the overall risk to the general public is low. It is usually a mild self-limiting illness, and most people recover within a few weeks. However, severe illness can occur in some individuals.
“Initial symptoms of monkeypox include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion.”
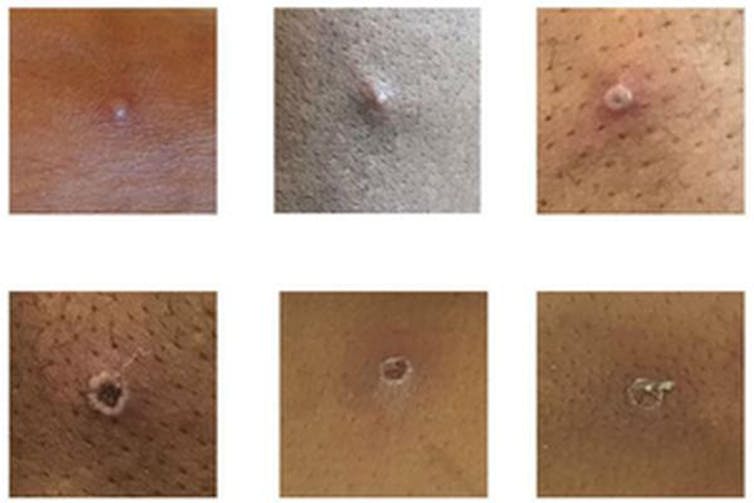
“A rash can develop, often beginning on the face, then spreading to other parts of the body, particularly the hands and feet.”
“The rash changes and goes through different stages before finally forming a scab, which later falls off.”
“Everyone is being asked to be aware of the monkeypox symptoms, but it is important that gay and bisexual men are alert as it’s believed to be spreading in sexual networks.”
“Anyone with unusual rashes or lesions on any part of their body should contact NHS 111 or call a sexual health service if they have concerns.”
Cases of monkeypox in the UK, including in Wales, are reported on the UKHSA website.
How is monkeypox spreading?
The first patient in the current outbreak had returned to the UK from travels to Nigeria where monkeypox is endemic.
However, cases are now spreading among people who have not travelled to west or central Africa, suggesting local transmission is occurring.
Monkeypox usually spreads by close contact and respiratory droplets.
What are the symptoms?
Early symptoms are flu-like, such as a fever, headaches, aching muscles and swollen lymph nodes.
Once the fever breaks, a rash can develop, often beginning on the face and then spreading to other parts of the body – most commonly the palms of the hands and soles of the feet.
How deadly is monkeypox?
Monkeypox is mostly a mild, self-limiting disease lasting two-to-three weeks. However, in some cases, it can cause death. According to the WHO, the fatality rate “in recent times” has been around 3% to 6%. The west African monkeypox virus is considered to be milder than the central African one.
Monkeypox tends to cause more serious disease in people who are immunocompromised – such as those undergoing chemotherapy – and children. There have been no deaths from monkeypox in the current worldwide outbreak, but, according to the Daily Telegraph, one child in the UK is in intensive care with the disease.
Why is it called monkeypox?
Monkeypox was first identified in laboratory monkeys (macaques) in Denmark in 1958, hence the name. However, monkeys don’t seem to be the natural hosts of the virus. It is more commonly found in rats, mice and squirrels. The first case in humans was seen in the 1970s in the Democratic Republic of the Congo.
Is monkeypox related to smallpox and chickenpox?
Monkeypox is related to smallpox – they are both orthopoxviruses – but it is not related to chickenpox. Despite the name, chickenpox is a herpes virus, not a poxvirus. (How “chicken” got in the name is not entirely clear. In his dictionary of 1755, Samuel Johnson surmised that it is so named because it is “of no very great danger”.) Nevertheless, the vesicles (little pus-filled blisters) caused by monkeypox are similar in appearance to those of chickenpox.
Are cases likely to continue rising?
Cases are likely to continue to rise significantly over the next two-to-three weeks, but this is not another pandemic in the making. Monkeypox doesn’t spread anywhere near as easily as the airborne virus SARS-CoV-2 that causes COVID-19.
Has monkeypox evolved to be more virulent?
RNA viruses, such as SARS-CoV-2, don’t have the ability to check their genetic code for mistakes each time they replicate, so they tend to evolve faster. Monkeypox is a DNA virus, which does have the ability to check itself for genetic mistakes each time it replicates, so it tends to mutate a lot slower.
The first genome sequence of the current outbreak (from a patient in Portugal) suggests that the virus is very similar to the monkeypox strain that was circulating in 2018 and 2019 in the UK, Singapore and Israel. So it is unlikely that the current outbreak is the result of a mutated virus that is better at spreading.
How is monkeypox diagnosed?
In the UK, swab samples taken from the patient are sent to a specialist laboratory that handles rare pathogens, where a PCR test is run to confirm monkeypox. The UK Health Security Agency has only one rare and imported pathogens laboratory.
Is there a vaccine for it?
Vaccines for smallpox, which contain the lab-made vaccinia virus, can protect against monkeypox. However, the vaccine that was used to eradicate smallpox can have severe side-effects, killing around one in a million people vaccinated.
The only vaccine specifically approved for monkeypox, Imvanex, is made by a company called Bavarian Nordic. It uses a nonreplicating form of vaccinia, which causes fewer side-effects. It was approved by the US Food and Drug Administration and the European Medicines Agency in 2019 – but only for use in people 18 years of age or older.
UK health secretary Sajid Javid said that the UK government will be stocking up on vaccines that are effective against monkeypox. The UK currently has about 5,000 doses of smallpox vaccine, which has an efficacy of around 85% against monkeypox.
Are there drugs to treat it?
There are no specific drugs to treat monkeypox. However, antivirals such as cidofovir and brincidofovir have been proven to be effective against poxviruses in animals and may also be effective against monkeypox infections in humans.
[Image and Q&A republished from The Conversation under a Creative Commons license. Read the original article.]
Health
Doctor struck off after sexual misconduct findings at Withybush Hospital

Tribunal history reveals medic was removed in 2012 for dishonesty before being allowed back to practise
A DOCTOR accused of sexually harassing junior colleagues while working at Withybush Hospital had previously been struck off the medical register for lying about his qualifications, the Herald can reveal.
Dr Velmurugan Kuppuswamy is currently at the centre of fitness-to-practise proceedings after allegations he made sexually inappropriate comments and subjected two female doctors to unwanted physical contact during his time as a locum consultant in Haverfordwest.
But records show this is not the first time his conduct has come before regulators.
In 2012, an independent tribunal found he had been dishonest during an application and interview for a postgraduate cardiology training post at an NHS deanery in England.
The panel heard he falsely claimed to have submitted a Doctor of Medicine thesis, said he was a member of the Royal College of Physicians and stated he had passed a practical clinical skills assessment.
He initially admitted misleading information before later retracting parts of his account. The tribunal concluded he had “maintained his dishonest accounts” and had wrongly accused a witness of giving misleading evidence.
He was erased from the register and returned to India, where he later worked in a cardiac hospital.
In 2020, he applied to be restored to the UK medical register.
The General Medical Council investigated and opposed the application, arguing his expressions of remorse had come years late and raising concerns about a lack of independent evidence regarding his work overseas, as well as the absence of relevant ethics training.
However, an independent Medical Practitioners Tribunal at the Medical Practitioners Tribunal Service accepted his assurances that he had changed. His evidence was described as “compelling, heartfelt and genuine”, and the panel decided a well-informed member of the public would not be concerned about his return to practise.
His name was restored to the register.
Shortly afterwards, he began working shifts as a locum consultant at Withybush Hospital, which is run by Hywel Dda University Health Board.
Within months, fresh allegations emerged.
A tribunal has heard claims that between August and September 2021 he hugged junior colleagues without consent, touched their backs and waists, squeezed their wrists and arms and made sexually suggestive remarks at a staff social event.
On two occasions, he is alleged to have gripped one doctor so tightly it caused pain and ignored her requests to stop. He is also accused of staring at female colleagues, following groups of women around the venue, making comments about their bodies and placing a hand high on one doctor’s thigh.
Further allegations relate to behaviour at work, including sitting extremely close to a colleague, draping an arm behind her on a sofa and grabbing her arm while whispering comments.
According to the charges, his conduct created “an intimidating, hostile, degrading, humiliating or offensive environment” and amounted to a sexually motivated abuse of his senior position.
Dr Kuppuswamy denies wrongdoing.
Following the investigation, the case was referred to a tribunal by the General Medical Council. The decision on his fitness to practise was made independently by a Medical Practitioners Tribunal at the Medical Practitioners Tribunal Service.
The tribunal determined his behaviour amounted to serious professional misconduct and ordered that he be erased from the medical register.
Asked whether the doctor remains employed, the health board said it does not comment on individual staffing matters.
Medical director Mark Henwood said: “We have robust policies and procedures in place to ensure the safety of both staff and patients in our care and we take seriously our responsibility for their wellbeing. We are committed to providing a safe, supportive environment where patients and staff can be confident that best practice is being followed at all times.”
Health
‘Parking fine or miss my appointment’ say patients pressure mounts at hospitals

From sleeping on chairs to parking fines, patients say everyday barriers are pushing the NHS to breaking point
PATIENTS across West Wales are describing a health service under such strain that some say they now expect to be penalised simply for trying to access care.
At Glangwili Hospital, stories of patients sleeping on chairs for days due to a lack of beds have been accompanied by growing frustration over issues that begin long before anyone reaches a ward — including parking, access, and the sheer difficulty of getting through the hospital doors.
One disabled patient said they had resigned themselves to receiving a £25 parking fine in order to attend hospital appointments.
“I now accept I will be fined,” they said. “Parking is impossible, but it’s that or miss my appointment. I am too disabled to park miles away and the disabled spaces are always full.”
Others have described spending days in A&E or side rooms, unable to lie down, while waiting for a bed to become available. One patient admitted on New Year’s Day with pneumonia said they slept in a chair for four nights without a pillow or blanket before being moved, only to later discover they also had flu and should have been isolated sooner.
Across social media and in correspondence with the Herald, patients and families repeatedly stress that frontline NHS staff are not to blame — instead pointing to a system that they say is buckling under years of structural strain.
Glangwili, the largest hospital managed by Hywel Dda University Health Board, serves Carmarthenshire and is home to the county’s only accident and emergency department following the closure of A&E at Prince Philip Hospital. That closure, along with reductions in services elsewhere, is frequently cited by patients as a turning point.
Several people said the loss of local A&E and cottage hospitals has forced more patients into already stretched units, increasing ambulance reliance and long-distance travel — particularly difficult in a largely rural region.
Further west, uncertainty over services at Withybush Hospital continues to fuel anxiety, especially given the scale of reinforced autoclaved aerated concrete (RAAC) identified across the site.
Hywel Dda has acknowledged that almost 90% of Withybush is affected by RAAC, while Glangwili itself is the oldest acute hospital in Wales. The health board says more than £50 million has been spent on the two hospitals in recent years, largely to address critical safety and infrastructure risks rather than expand capacity.
Patients, however, question where that money is felt on the ground.
Some have criticised NHS procurement and management structures, while others point to social care as the missing piece. Repeated comments highlight the lack of care packages and closed care homes, which many believe are leaving medically fit patients unable to be discharged — effectively blocking beds and creating bottlenecks throughout the system.
“There’s nowhere for people to go,” one reader said. “Until social care is sorted, nothing will change.”
Concerns have also been raised about staff morale, with some alleging bullying cultures and burnout contributing to recruitment and retention problems. Again, blame is consistently directed upward rather than at nurses, doctors or porters.
Behind it all looms the long-promised new ‘super hospital’ for Carmarthenshire — first discussed in 2006 and formally launched in 2018. Eight years on, construction has yet to begin, and public confidence in the project is fading.
While Hywel Dda and the Welsh Government insist improvements are under way — including additional funding to expand capacity at Glangwili and improvements to patient experience — many patients say their reality feels far removed from official assurances.
For those attending appointments, sleeping in chairs, or weighing up a parking fine against missing care, the crisis is no longer abstract.
“It’s not politics,” one patient said. “It’s whether you get treated — and how.”
Health
Consultation reveals lack of public trust in health board

EARLIER this week, Hywel Dda UHB published the results of a consultation into the future configuration of its clinical services.
It is widely accepted that the current provision of clinical services is unsustainable. The Board cannot recruit enough staff to fill vacancies, particularly in rural areas, despite the existing staff shortages there. Only Prince Philip Hospital in Llanelli, situated close to the medical faculty and research facilities in Swansea, experiences relatively little difficulty recruiting and retaining staff.
A QUESTION OF TRUST
Public reactions online to the publication of the results, particularly in Pembrokeshire, were plentiful and mostly negative. Those initial reactions were predictable, even where the report’s details had not been read. However, an examination of the consultation’s findings paints a troubling picture for the Board.
Many of the approximately 4,000 respondents to the consultation said they understood the practical difficulties of delivering healthcare across rural Wales with limited resources. However, many also said they did not expect the Health Board to act in good faith upon its findings. Using the definition of ‘many’ adopted by ORS, a slight majority of respondents to the consultation said, in terms, that they did not trust their local health board.
We asked the Health Board to respond to those findings.
The Board told us: “We hope that by giving the people and communities in Hywel Dda the chance to share their views, we can work together on planning for the future of health care that is safe, accessible, sustainable and kind. More than 4,000 people engaged with us by attending our events, held throughout the Hywel Dda area, neighbouring Health Boards, and online.
“At the Extraordinary Board meeting on the 18 and 19 February, the Board will be considering 48 options across the nine services, 22 of which are alternative options generated directly through staff, public and stakeholder feedback during the consultation process. This reflects our genuine commitment to listening to our communities. There are no preferred options.”

THE ROAD AHEAD
The consultation report included a large range of responses expressing serious concerns about access to services close to home. Respondents aired even stronger misgivings about the linked issue of transport for those attending hospital appointments. Simply put, options that proposed centralising services in one centre or another met with almost universal short shrift from the public.
The options proposed by the Board contained no hint of a transport assessment if key services were centralised, particularly from rural areas. Concerns about transport links, a bugbear for respondents from Pembrokeshire, were expressed by members of the public living in Ceredigion, in rural Carmarthenshire east and north of the M4 and A40.
Without a massive investment in patient transport services or a massively expanded public transport system, it is difficult to see how the Board could reasonably expect a patient with a debilitating condition to reach an appointment many miles away. Therefore, we asked the Board what transport it had commissioned to justify and underpin the options in the consultation.
The Board said: “We carried out Equality Impact Assessment (EqIA) and Quality Impact Assessment (QIA) during options development. Alongside this, there is a dedicated Patient and Travel Insights assessment to explore how changes could affect journeys and access to care. This includes analysis of travel times, transport patterns and the potential effects on different groups.
“We have carefully considered how proposed changes to healthcare services could impact travel and transport for patients, loved ones, and our staff. Some options may involve longer travel times for some people to ensure they can access better-quality care. We have worked with partners such as the Welsh Ambulance Service, the University NHS Trust, and the Adult Critical Care Transfer Service to ensure appropriate transport arrangements have been considered.
“We will continue to work with partners to understand how we can reduce the impact of any changes on travel and transport.”
A DIGITAL FUTURE?
This is at least the fourth consultation this reporter has reported on in the last eleven years. Each has suggested the future provision of healthcare services through technological solutions.
If patients must travel further for appointments, many of which will be clinically routine, remote medical appointments would go some way to addressing that issue. On the surface, it’s a win-win.
Progress has been slow. The technical demands of remote consultation and creaking IT infrastructure have delayed rollout. The risks attendant upon assessing a patient’s condition over a videolink remain undiminished. Moreover, a significant number of older patients either cannot or will not access services online. Rural broadband roll-out, which remains piecemeal, has not been the cure-all previously imagined.
We asked how the options accounted for the factors listed above.
The Board’s response stated that: “Digital is increasingly becoming the means by which we all interact with each other and with everything around us. However, we understand that some members of our Hywel Dda population cannot always access services online, or prefer not to, and we will support them in accessing healthcare in the way that is most convenient for them.”

FINDING (AND KEEPING) STAFF
The problems west Wales has in attracting and retaining healthcare staff are well known. They are chronic and, despite numerous initiatives, have not gone away. Rural areas are a hard sell to young professionals, especially those ambitious to specialise in cutting-edge practice areas. All principal research centres are based in or close to cities. In South Wales, that means Swansea, Cardiff, and Bristol. It follows that the more distant a post is from those centres, the less likely an early-career professional will apply for it.
Meanwhile, working conditions, shift patterns, and travel times to and from workplaces, often miles from home, mean that agency working (less secure, but better paid and more flexible) is an attractive alternative to direct employment. Despite Welsh Government diktats to cut the use of agency staff, healthcare delivery operates in the real world.
The Board told us: “Staff recruitment and retention are challenges across the NHS, especially in rural areas. We continue to recruit staff by offering them competitive remuneration packages and excellent opportunities to work, train and progress in our hospitals and health sites.
“An important motivation for the CSP programme was the expectation that more sustainable, higher-quality services would be more attractive to staff, helping with both retention and recruitment.
“Some options seek to recruit more substantive staff rather than temporary staff, which will be better for our clinical teams and improve patient care. Some options provide current staff with chances to work more closely together in teams and offer more training opportunities.”

PEMBROKESHIRE FIGHTS FOR WITHYBUSH
Opposition to the options proposed by the Health Board was predictably strongest when it came to removing services from local hospitals. In Ceredigion, a 16,000-signature petition opposed the removal or reduction of stroke services at Bronglais. In Llanelli, an option to close the Emergency Care Unit drew a negative reaction. In Llandovery, the loss of radiology services garnered a similarly trenchant response. In particular, a large majority of responses rejected proposals to introduce a treat-and-transfer system.
Against that background, it is hardly surprising that Pembrokeshire respondents stood firmly against any further reduction in services provided in the county, and particularly at Withybush. Having experienced the salami-slicing of services away from Haverfordwest, and in the face of repeatedly broken assurances regarding the return of services ‘temporarily’ removed, those reactions are unsurprising. Those feelings are not limited to the public. One staff member was directly quoted in the consultation report claiming that cuts to Withybush were baked into the options the Board presented.
We asked the Board to provide specific reassurance about maintaining current service provision at Withybush and other Pembrokeshire hospitals.
Whether the Board’s response addresses that question, the reader can decide.
“Withybush Hospital will have an important role to play in the health care of the region, and our long-term plan for our hospital sites has been set out in our A Healthier Mid and West Wales strategy. In the interim, our CSP consultation has included our thinking on the role of each of our acute sites. For example, we anticipate that Withybush Hospital will provide more planned care, and initial access to acute care would remain on site, with transfers to Glangwili Hospital for patients with the highest needs.”

PEMBROKESHIRE MSs RESPOND
Local Welsh Conservative Senedd Members Paul Davies MS and Samuel Kurtz MS have warned that any decision which undermines the future of A&E services at Withybush Hospital would be “wholly unacceptable”, ahead of a crucial Hywel Dda University Health Board meeting in February.
Paul Davies MS, joined by fellow Welsh Conservative Senedd Member Samuel Kurtz MS, said Withybush Hospital must be protected as a vital lifeline for Pembrokeshire, and that communities are deeply concerned about the potential consequences of the Health Board’s proposals.
Paul Davies MS said: “People in Pembrokeshire are deeply worried about what these proposals could mean for Withybush Hospital. Over many years, we have seen a gradual erosion of services, and communities are understandably anxious that this process will continue.
“Withybush Hospital is not a ‘nice to have’ — it is a vital lifeline for a large, rural population. Any changes must strengthen services in Pembrokeshire, not weaken them. I will not support decisions that place patients at greater risk or force them to travel unreasonable distances for essential care.”

Samuel Kurtz MS added, “People in Pembrokeshire have heard this story before. Time and again, we are told services are fragile, and the result is that Withybush loses out.
“The loss of SCBU, consultant-led maternity and children’s A&E is still deeply felt locally. Removing one service often makes others unviable, and that is exactly what people are worried about now.
“Any decision that threatens the long-term viability of A&E at Withybush Hospital is a red line. It would be wholly unacceptable and would be met with fierce opposition from the community.”
Mr Kurtz also stressed that rurality, transport challenges and ambulance pressures must be central to decision-making, not treated as secondary considerations.
“Pembrokeshire is a rural county. Asking patients to travel further for emergency or urgent care is not a theoretical issue — it affects safety, outcomes, families and staff.
He continued: “There is also deep frustration that these decisions continue to be made in the shadow of the so-called ‘super hospital’ elsewhere in west Wales, which has never come to fruition. Pembrokeshire cannot be left with a slow erosion of services while waiting for something that may not materialise for a decade or more.”
Both Senedd members have written to Hywel Dda University Health Board and the Welsh Government ahead of the February meeting.
Paul Davies MS concluded: “We will be watching the outcome of this meeting very closely. Withybush Hospital is vital to Pembrokeshire. It must be properly supported, not hollowed out.”
-

 Health6 days ago
Health6 days agoConsultation reveals lack of public trust in health board
-

 News7 days ago
News7 days agoCaldey still unsafe, survivors warn — despite Abbey’s reform claims
-

 Community7 days ago
Community7 days agoPembrokeshire students speak at national Holocaust Memorial Day event
-

 News19 hours ago
News19 hours agoPrincess of Wales visits historic Pembrokeshire woollen mill
-

 News7 days ago
News7 days agoKurtz raises Gumfreston flooding in the Senedd as petition deadline nears
-

 Crime5 days ago
Crime5 days agoPembroke man accused of child sex offences sent to Swansea Crown Court
-

 Education7 days ago
Education7 days ago‘Vulnerable teen’ questioned by police at Milford Haven School
-

 Education7 days ago
Education7 days agoAttendance concerns at Milford School reflect wider issue raised at the Senedd





























