Health
Locked up for Autism: Thousands detained under mental health law

“He didn’t break the law. He just needed help. Now he’s locked in a hospital hundreds of miles away.” — Alun, father of a detained 19-year-old
IN SECURE hospitals across England and Wales, more than 2,000 people with autism or learning disabilities remain locked away under mental health laws — despite never committing a crime.
Many are detained under the Mental Health Act 1983, often after being taken by police during a mental health crisis. The vast majority have no mental illness diagnosis. Some are teenagers. A few have been there for decades.
“It’s a human rights scandal,” said Dan Scorer of Mencap. “They’re being institutionalised because society hasn’t built the support they need.”
Autism is not a mental illness. It is widely recognised that for most autistic people, care in an inpatient unit is rarely helpful – in fact, it can be deeply damaging.
The average length of stay is around 4.6 years.
The overwhelming majority (92%) of autistic people and people with a learning disability who are detained in hospitals are put there using the Mental Health Act of 1983.
A NEED FOR URGENT REFORM
For years, the National Autistic Society and tens of thousands of campaigners have called for changes to mental health law.
Reform has been promised, and a bill is making its way through Parliament. However, the government will not commit to funding the reforms the legislation will enact. Even then, campaigners say the law change will not end the scandal of detention.
In April, Denise Cavanagh from Hook, a founder of the Stolen Lives campaign, told BBC Wales that she believed people would still be detained via other laws, including the Mental Capacity Act.
She added: “People with learning disabilities often end up in hospitals because there’s a breakdown in housing and community care, and it’s the only place they can go.
“So, if that community care isn’t there, there is nowhere for them to go and they’ll still be detained.”
And even though health is devolved to Wales, the Welsh Government is relying on a Westminster bill to improve how people with learning disabilities and autism are supported during a crisis.
“THEY CAME WITH HANDCUFFS”
Michelle, from Wiltshire, recounts the day her autistic daughter was detained after a meltdown in a supermarket.
“She was 23. She was overwhelmed. She panicked. That’s all. But the police came and took her away. That was three years ago. She hasn’t been home since.”
Michelle’s story is one of many. Some families describe wards where patients are sedated, isolated, and cut off from loved ones.
Bethany – whose surname cannot be published – was locked in a hospital room in Northampton as a teenager. Her only access to the outside world was through a tiny hatch in the door.
Her father, Jeremy, said he could only see his daughter through a plastic screen or through the six-inch hatch.
“It was cruel. It was torture for my daughter,” he said.
“It broke her human rights, her right to family life, her right to freedom from degrading treatment.”
Even now, several years on from Jeremy’s interview on Radio Four regarding Bethany’s treatment, little has changed. In fact, the data shows a worrying trend towards increased detention of those with mental illness or specific learning difficulties.
NO WAY OUT
Official NHS data reveals the extent of the crisis:
Over 52,000 people were detained under the Mental Health Act in April 2024 — the highest figure in five years.
Over 2,000 of those are autistic or have a learning disability.
As of May 2025, 2,025 autistic people and people with a learning disability are in mental health hospitals in England. Of these, 1,455 (72%) are autistic.
There are 240 under-18s in inpatient units who are autistic or have a learning disability. Of these, 230 (96%) are autistic.
The number of autistic people without a learning disability detained in mental health hospitals has increased by 141% since 2015.
This is the most up-to-date record of how many autistic people and people with a learning disability are currently in mental health hospitals in England.
Despite some progress moving people with a learning disability out of hospitals and into the community, the number of autistic people detained has increased. In 2015, autistic people made up 38% of the total number in hospitals, now it is 72%.
Around 60% of learning disability or autism inpatients have no mental illness diagnosis.
Detained patients are often placed in “out-of-area” units, sometimes hundreds of miles from home.
Toni Dymond, an autistic woman, was detained for over 20 years in psychiatric care without a criminal charge.
“She was isolated, broken,” said her brother in a statement. “It wasn’t treatment. It was abandonment.”
34,685 people were detained by police under Section 136 of the Mental Health Act in 2022–23.
Over 60% were transported in police vehicles, not ambulances.
Autistic woman and author of the memoir Unbroken, Alexis Quinn, spent three years “locked inside” various mental health hospitals, including Assessment and Treatment Units (ATU).
She says: “I was detained under the Mental Health Act and remained so for most of my stay. The Mental Health Act is a piece of legislation which provides a legal framework to detain people when they are mentally ill and require treatment to get better. The interesting thing about a treatment order for an autistic person is that autism is not a mental health condition.
“Whilst mental illnesses, such as depression and anxiety, can be treated, for autistic people, this has to be done in a way that reflects their needs and understands autism.
“When I was detained under the Mental Health Act, I felt like this was because of behaviour relating to my autism, not because I was mentally ill; the whole process lacked any understanding of the difference between autism and mental illness.”
CHANGE PROMISED, BUT NO MONEY ON THE TABLE
The Mental Health Bill, which is currently going through Parliament, will stop people with a learning disability and autistic people from being detained for treatment. However, the government have said that this change to the law will not be enforced until there is sufficient community support. That means the law will not come into effect until there are enough resources to support its operation. There is no commitment to provide that funding.
The Challenging Behaviour Foundation, a national charity, wants a clear plan, co-produced with people with lived experience, families, and those working within the different parts of the system, setting out what steps will be taken to develop this support and accompanied by the resources to make it happen.
The National Autistic Society says: “We are calling on the government to urgently publish a comprehensive and fully-costed plan for how it intends to build this support.”
So far, that call has been met with silence.
Health
Nurses warn of pay and burnout crisis as new report exposes pressures in Wales
A NEW national report has laid bare the growing pressures facing nurses and midwives in Wales, with concerns over pay, burnout and lack of professional development threatening the long-term future of the workforce.
The findings, published by the Nursing and Midwifery Council in its Spotlight on Nursing and Midwifery 2025 report, show that while many nurses remain deeply committed to their roles, large numbers feel undervalued, overstretched and reluctant to recommend the profession to others.
Responding to the report, Royal College of Nursing Wales said the data should act as a wake-up call for government and health boards.
Professor Sandy Harding, Associate Director of Nursing, Policy and Professional Development at RCN Wales, said:
“We welcome the determination and commitment shown by our existing nurses in Wales, with more than half surveyed saying they are satisfied with their day-to-day work and motivated by making a difference to people’s lives. However, the findings also present a stark reflection of the poor health of nursing in Wales.
“Too many nurses are not recommending the profession to others, are struggling and are facing abuse and discrimination in the workplace.”
Pay falling behind responsibility
One of the most pressing concerns raised in the report is pay.
Nursing leaders say salaries have failed to keep pace with the growing complexity of the job, heavier caseloads and the rising cost of living, leaving many staff feeling undervalued and financially squeezed.
For some, the pressure is forcing difficult decisions about staying in the profession or reducing hours.
RCN Wales argues that without meaningful improvements to pay, recruitment and retention will continue to suffer, placing further strain on already stretched hospital wards, community services and care settings.
Training and career progression gaps
The report also highlights inconsistent access to continuing professional development, with many nurses struggling to secure protected time or funding for further training.
According to the union, this not only limits career progression but risks undermining patient care in the long term.
Harding said: “Access to protected time and funding for continuing professional development remains inconsistent, undermining both career progression and the sustainability of the workforce.
“RCN Wales believes this is unacceptable and we will continue to support nurses and fight for fair pay, meaningful investment in professional development and better working conditions across Wales.”
Commitment remains strong
Despite the challenges, the report does note strong dedication among nursing staff.
More than half of those surveyed said they were satisfied with their day-to-day work and remained motivated by the difference they make to patients’ lives.
Health leaders say that commitment is a strength the NHS in Wales cannot afford to lose.
With around 35,000 members in Wales, the Royal College of Nursing says it will continue pressing ministers to address what it describes as a “workforce crisis” before it deepens further.
The union is calling for fairer pay settlements, safer staffing levels and guaranteed investment in training to ensure nursing remains an attractive and sustainable career.
Health
Doctor struck off after sexual misconduct findings at Withybush Hospital

Tribunal history reveals medic was removed in 2012 for dishonesty before being allowed back to practise
A DOCTOR accused of sexually harassing junior colleagues while working at Withybush Hospital had previously been struck off the medical register for lying about his qualifications, the Herald can reveal.
Dr Velmurugan Kuppuswamy is currently at the centre of fitness-to-practise proceedings after allegations he made sexually inappropriate comments and subjected two female doctors to unwanted physical contact during his time as a locum consultant in Haverfordwest.
But records show this is not the first time his conduct has come before regulators.
In 2012, an independent tribunal found he had been dishonest during an application and interview for a postgraduate cardiology training post at an NHS deanery in England.
The panel heard he falsely claimed to have submitted a Doctor of Medicine thesis, said he was a member of the Royal College of Physicians and stated he had passed a practical clinical skills assessment.
He initially admitted misleading information before later retracting parts of his account. The tribunal concluded he had “maintained his dishonest accounts” and had wrongly accused a witness of giving misleading evidence.
He was erased from the register and returned to India, where he later worked in a cardiac hospital.
In 2020, he applied to be restored to the UK medical register.
The General Medical Council investigated and opposed the application, arguing his expressions of remorse had come years late and raising concerns about a lack of independent evidence regarding his work overseas, as well as the absence of relevant ethics training.
However, an independent Medical Practitioners Tribunal at the Medical Practitioners Tribunal Service accepted his assurances that he had changed. His evidence was described as “compelling, heartfelt and genuine”, and the panel decided a well-informed member of the public would not be concerned about his return to practise.
His name was restored to the register.
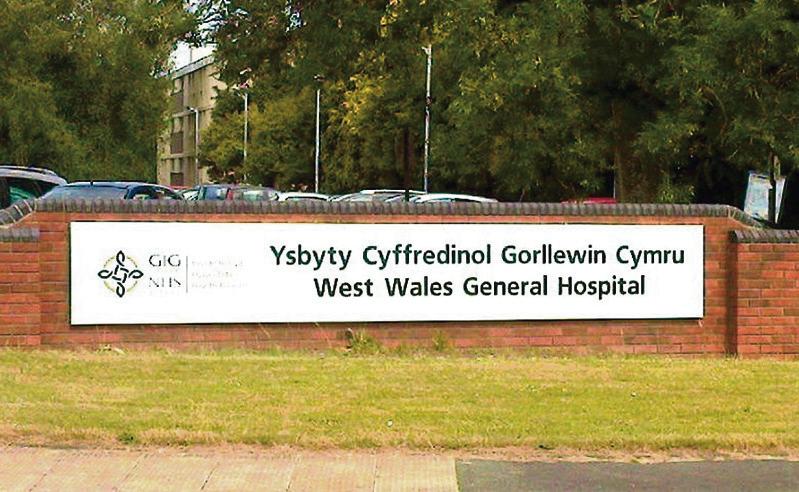
Shortly afterwards, he began working shifts as a locum consultant at Withybush Hospital, which is run by Hywel Dda University Health Board.
Within months, fresh allegations emerged.
A tribunal has heard claims that between August and September 2021 he hugged junior colleagues without consent, touched their backs and waists, squeezed their wrists and arms and made sexually suggestive remarks at a staff social event.
On two occasions, he is alleged to have gripped one doctor so tightly it caused pain and ignored her requests to stop. He is also accused of staring at female colleagues, following groups of women around the venue, making comments about their bodies and placing a hand high on one doctor’s thigh.
Further allegations relate to behaviour at work, including sitting extremely close to a colleague, draping an arm behind her on a sofa and grabbing her arm while whispering comments.
According to the charges, his conduct created “an intimidating, hostile, degrading, humiliating or offensive environment” and amounted to a sexually motivated abuse of his senior position.
Dr Kuppuswamy denies wrongdoing.
Following the investigation, the case was referred to a tribunal by the General Medical Council. The decision on his fitness to practise was made independently by a Medical Practitioners Tribunal at the Medical Practitioners Tribunal Service.
The tribunal determined his behaviour amounted to serious professional misconduct and ordered that he be erased from the medical register.
Asked whether the doctor remains employed, the health board said it does not comment on individual staffing matters.
Medical director Mark Henwood said: “We have robust policies and procedures in place to ensure the safety of both staff and patients in our care and we take seriously our responsibility for their wellbeing. We are committed to providing a safe, supportive environment where patients and staff can be confident that best practice is being followed at all times.”
Health
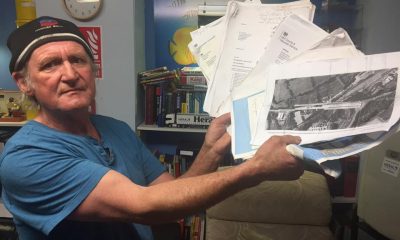
‘Parking fine or miss my appointment’ say patients pressure mounts at hospitals
From sleeping on chairs to parking fines, patients say everyday barriers are pushing the NHS to breaking point
PATIENTS across West Wales are describing a health service under such strain that some say they now expect to be penalised simply for trying to access care.
At Glangwili Hospital, stories of patients sleeping on chairs for days due to a lack of beds have been accompanied by growing frustration over issues that begin long before anyone reaches a ward — including parking, access, and the sheer difficulty of getting through the hospital doors.
One disabled patient said they had resigned themselves to receiving a £25 parking fine in order to attend hospital appointments.
“I now accept I will be fined,” they said. “Parking is impossible, but it’s that or miss my appointment. I am too disabled to park miles away and the disabled spaces are always full.”
Others have described spending days in A&E or side rooms, unable to lie down, while waiting for a bed to become available. One patient admitted on New Year’s Day with pneumonia said they slept in a chair for four nights without a pillow or blanket before being moved, only to later discover they also had flu and should have been isolated sooner.
Across social media and in correspondence with the Herald, patients and families repeatedly stress that frontline NHS staff are not to blame — instead pointing to a system that they say is buckling under years of structural strain.
Glangwili, the largest hospital managed by Hywel Dda University Health Board, serves Carmarthenshire and is home to the county’s only accident and emergency department following the closure of A&E at Prince Philip Hospital. That closure, along with reductions in services elsewhere, is frequently cited by patients as a turning point.
Several people said the loss of local A&E and cottage hospitals has forced more patients into already stretched units, increasing ambulance reliance and long-distance travel — particularly difficult in a largely rural region.
Further west, uncertainty over services at Withybush Hospital continues to fuel anxiety, especially given the scale of reinforced autoclaved aerated concrete (RAAC) identified across the site.
Hywel Dda has acknowledged that almost 90% of Withybush is affected by RAAC, while Glangwili itself is the oldest acute hospital in Wales. The health board says more than £50 million has been spent on the two hospitals in recent years, largely to address critical safety and infrastructure risks rather than expand capacity.
Patients, however, question where that money is felt on the ground.
Some have criticised NHS procurement and management structures, while others point to social care as the missing piece. Repeated comments highlight the lack of care packages and closed care homes, which many believe are leaving medically fit patients unable to be discharged — effectively blocking beds and creating bottlenecks throughout the system.
“There’s nowhere for people to go,” one reader said. “Until social care is sorted, nothing will change.”
Concerns have also been raised about staff morale, with some alleging bullying cultures and burnout contributing to recruitment and retention problems. Again, blame is consistently directed upward rather than at nurses, doctors or porters.
Behind it all looms the long-promised new ‘super hospital’ for Carmarthenshire — first discussed in 2006 and formally launched in 2018. Eight years on, construction has yet to begin, and public confidence in the project is fading.
While Hywel Dda and the Welsh Government insist improvements are under way — including additional funding to expand capacity at Glangwili and improvements to patient experience — many patients say their reality feels far removed from official assurances.
For those attending appointments, sleeping in chairs, or weighing up a parking fine against missing care, the crisis is no longer abstract.
“It’s not politics,” one patient said. “It’s whether you get treated — and how.”
-

 Health6 days ago
Health6 days agoConsultation reveals lack of public trust in health board
-

 News1 day ago
News1 day agoPrincess of Wales visits historic Pembrokeshire woollen mill
-

 Crime5 days ago
Crime5 days agoPembroke man accused of child sex offences sent to Swansea Crown Court
-

 Community7 days ago
Community7 days agoCampaign to ‘save’ River Cleddau hits over 2,200 signatures
-

 Health3 days ago
Health3 days agoDoctor struck off after sexual misconduct findings at Withybush Hospital
-
 Crime1 day ago
Crime1 day agoHakin man’s appeal delayed again as Crown Court seeks guidance on insurance law
-

 Community5 days ago
Community5 days ago50s women threaten legal action over pension compensation refusal
-

 Crime5 days ago
Crime5 days agoManhunt intensifies after woman seriously injured in Carmarthen park stabbing